An estimated 10 million people in the UK live with the daily challenge of arthritis—and for many, the condition feels noticeably worse in winter.
Whether the temperature drop is nudging joints to ache more fiercely or making movement a bit tougher, there are practical ways to find relief and keep doing what you love.
Despite how frequently we use the term, “arthritis” isn’t one single disease. It’s actually an umbrella for around 100 related joint conditions, and it can manifest in many forms—from osteoarthritis, where protective cartilage in the joints wears away, to autoimmune types like rheumatoid arthritis.
“The word ‘arthritis’ literally means inflammation of a joint,” says Dr. Sarah Brewer, Medical Director at Healthspan.
“The most common type, osteoarthritis, happens when the protective cartilage at the ends of your bones wears away.”
Without this cushion, tendons and ligaments face extra strain, sometimes resulting in painful bone-on-bone rubbing, swelling, and inflammation.
Other forms of arthritis—including gout, psoriatic arthritis, and reactive arthritis—also come under this umbrella, and can affect people of all ages.
While osteoarthritis often hits the hips and knees, rheumatoid arthritis typically has more widespread effects, causing severe stiffness and inflammation that may feel especially intense in the mornings.
Spotting the Symptoms

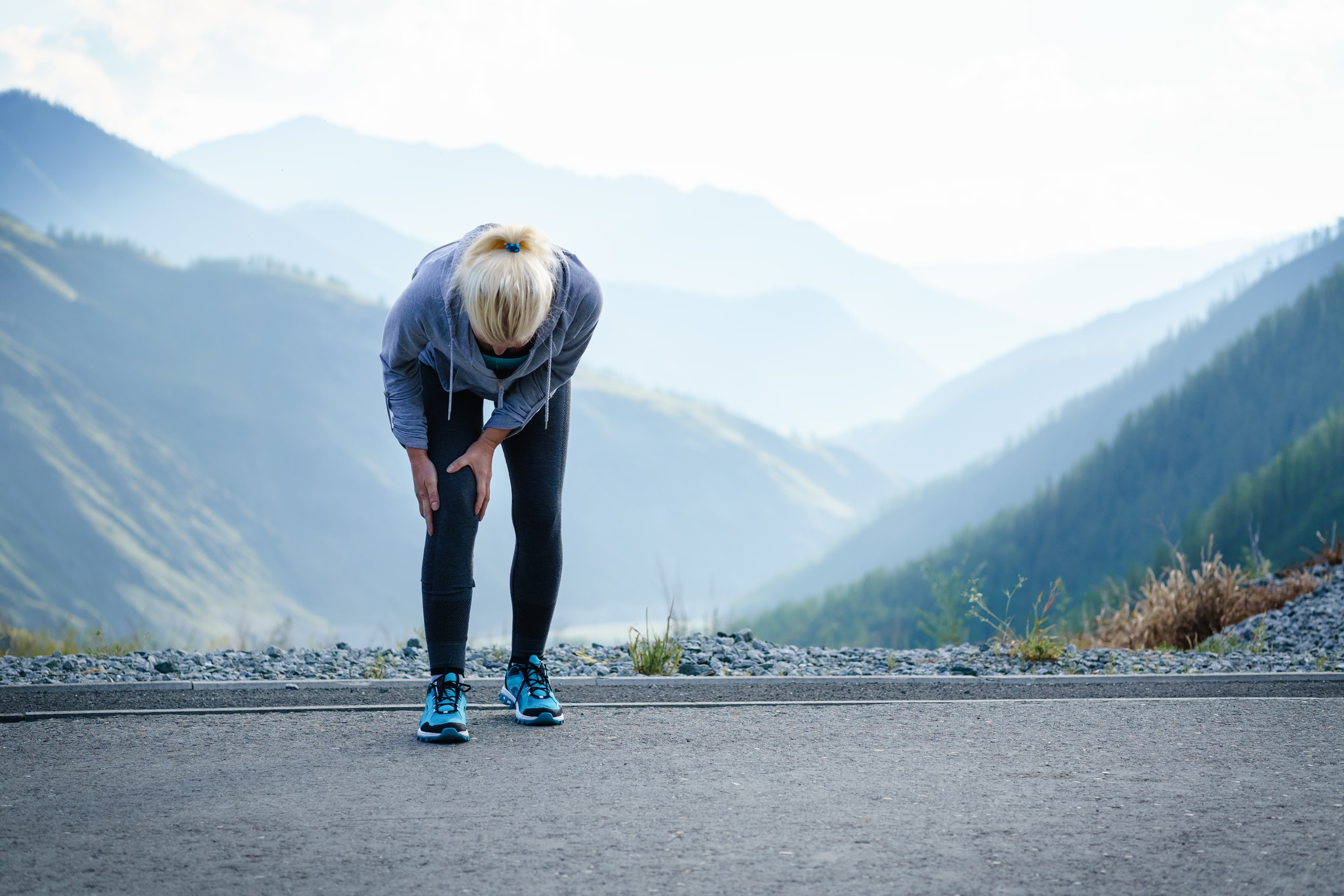
One of the earliest signs of osteoarthritis is pain—a dull ache or a burning sensation that worsens after using the affected joint.
Swelling, stiffness, and discomfort are common hallmarks as well, and over time, this inflammation may change how your joints look and function.
Different types of arthritis can overlap in symptoms, but doctors can usually narrow down the specific cause by noting which joints are affected, how quickly symptoms appear, and whether other issues—like eye inflammation or internal organ problems—are involved.
Why Does It Feel Worse in Winter?

For a significant number of people, the colder months seem to intensify the pain of arthritis. “Cold weather appears to make arthritis pain worse for many individuals, although the exact reason is not fully understood,” says Dr. Brewer.
In one small study of people with osteoarthritis or rheumatoid arthritis, 92% believed that low temperatures aggravated their discomfort, a finding backed by meteorological data charting pain levels against chilly forecasts.
Lower vitamin D levels in winter and heightened sensitivity of pain receptors in cold conditions are two possible explanations.
Ways to Ease Winter Flare-Ups

1. Stay Warm
Layer up to protect your most vulnerable joints and limit stiffness. Insulated clothing, knee supports, and gloves can all help maintain that crucial heat.
2. Explore Pain Relief Options
While oral painkillers like paracetamol and NSAIDs can be effective, Dr. Brewer warns about potential side effects with long-term use.
“Topical creams and gels that target the affected area directly are increasingly popular,” she explains. If in doubt, check with your GP for a tailored pain management plan.
3. Embrace Warm Water Therapy
Swimming in a heated pool can be a soothing, low-impact way to keep joints limber, while a warm bath before bed can offer calming relief that may also help with sleep.
4. Consider Supplements
“A number of supplements and herbal remedies may help reduce joint pain,” says Dr. Brewer. She suggests exploring options like glucosamine, chondroitin, hydrolysed collagen, ginger, turmeric, and krill oil. In particular, turmeric, taken in a solubilised liquid form, is known for better absorption.
Looking Ahead
Living with arthritis—even when it feels worse in winter—doesn’t mean you have to surrender to constant discomfort.
By layering up, exploring effective pain relief methods, and staying gently active (especially with warm water exercises), you can navigate the colder months with greater ease.
If you’re uncertain about which path to take, speak with a healthcare professional for personalised guidance.
Paying attention to your body’s cues and making small yet impactful changes can help keep those joints happier—even as the temperature dips. After all, winter might be chilly, but it doesn’t have to stop you from feeling your best.